How The Fear-Pain Cycle Is Keeping Your Pain Alive
Jan 05, 2026Read the blog post or watch the video-version on YouTube. You'll find both below!
If you live with IBS, chronic pain, or chronic physical symptoms, there is one mental habit that can quietly keep the problem going, even when nothing is structurally wrong in the body.
That habit is fear and worry about symptoms. Fear of pain. Fear of flare-ups. Fear that something is seriously wrong.
While this response is completely understandable, neuroscience shows that fear itself can intensify and prolong symptoms. In this article, you will learn why fear makes IBS and chronic pain worse, how the brain learns this pattern, and what you can do to start reversing it.
Why Fear and Worry Make Symptoms Worse
Fear is not just an emotional reaction. From the brain’s perspective, fear is a signal of danger. When symptoms appear and are met with worry or alarm, the nervous system becomes more alert. Over time, this heightened alertness can increase pain, digestive symptoms, and bodily tension rather than reduce them.
To understand why, we need to look at how the brain processes threat.
Your Brain Treats Emotional and Physical Threats the Same
The brain has one core job: to protect you. It constantly scans your internal and external environment for danger and asks a single question: “Is this dangerous?”
From the brain’s point of view, it does not matter whether a threat is physical or emotional. Brain imaging studies show that emotional pain and physical pain activate the same alarm systems. Fear, worry, rejection, and loss light up the same brain regions as bodily injury.
This means that fear about symptoms is processed as a real physical threat. When you worry about pain, digestion, or flare-ups, the brain does not interpret that as just a thought. It interprets it as danger.
Pain Is Created by the Brain, Not Directly by the Body
Pain does not come straight from the body. Instead, sensory signals travel from the body to the brain, the brain evaluates those signals and decides whether pain is necessary. Pain is a protective output, not a direct measurement of damage.
If the brain believes something is dangerous, it turns the pain signal up to get your attention. The fear sends a clear message to the brain: “This is dangerous. Pay attention.”
The brain responds by increasing symptoms such as pain, urgency, tension, or discomfort, not to harm you, but to protect you.
How the Pain–Fear Cycle Is Created
This process often turns into a self-reinforcing loop. It usually follows this pattern:
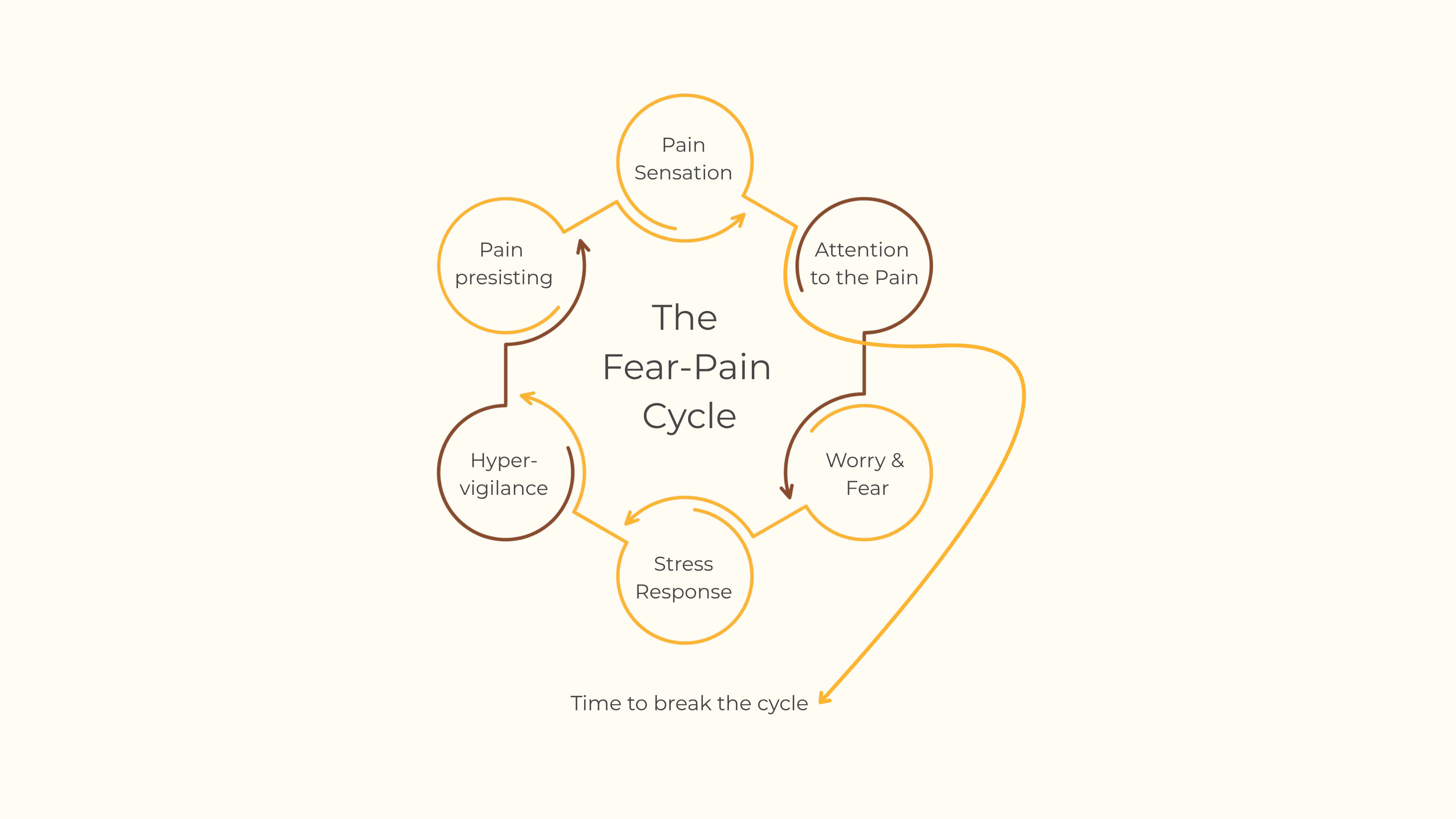 Over time, the brain starts to learn this loop. In neuroscience, this is often summarized as “neurons that fire together wire together.”
Over time, the brain starts to learn this loop. In neuroscience, this is often summarized as “neurons that fire together wire together.”
When pain and fear repeatedly occur together, the brain links them into a single automatic pattern. Eventually, pain will trigger fear, and fear will trigger more pain. This can happen even when there is no ongoing injury, inflammation, or disease.
This is what is known as neuroplastic pain. The pain is real, physical, and often intense, but it is maintained by learned brain circuits rather than tissue damage.
Why Safety Turns Pain Down
The opposite of fear is not force, control, or suppression. The opposite of fear is safety. When the brain feels safe, it has no reason to stay on high alert. Alarm signals quiet down, pain intensity naturally reduces, and pain improves not because it is fought or ignored, but because the brain updates its prediction from danger to safety.
This is why reducing fear reduces pain. Calm, confident responses weaken symptoms over time because they teach the brain that there is no emergency.
But How Do You Break the Cycle?
Breaking the pain–fear cycle does not start with positive thinking or pretending symptoms are not there. It starts with clarity and certainty.
Step 1: Rule Out Injury or Disease
Always begin with a proper medical evaluation. This step is essential. The brain cannot learn safety if there is still uncertainty about structural damage or disease.
Step 2: Check for Neuroplastic Pain Patterns
Once physical causes are ruled out, the next step is to assess whether your symptoms fit the pattern of neuroplastic pain. Common signs include:
- Symptoms that fluctuate without a clear physical cause
- Pain that spreads, shifts, or changes over time
- Symptoms that worsen with stress, fear, or attention
- Long-standing pain despite normal tests and scans
When you know your body is not damaged, you can respond to symptoms differently. Instead of fear, you respond with calm, confidence, and nonchalance. This teaches the brain that the symptoms are not important and not dangerous. Over time, the alarm system quiets down.
Fear is not a weakness, it's a signal that the brain is trying to protect you. The goal is not to fight fear, but to teach the brain that it no longer needs to be afraid. That is where real, lasting change begins.
A Free Neuroplastic Pain Assessment
To support this process, we have created a free assessment that can help you determine whether your symptoms are likely neuroplastic. You can find the link to the assessment here.
If this article resonates with you, or someone in your life, you can also learn more about working with us.
Join the Mind-Body Connection newsletter
Weekly newsletters on how you can retrain your brain, and break out of the cycle of fear and pain.
Our readers are our only priority. See our privacy policy at the bottom of the page.

